In the 2012 Australian Health Survey, it was reported that around 917,000 Australians had been diagnosed with diabetes…..this equates to a bit over 5% of the population! Type 2 diabetes, which is often referred to as adult onset diabetes, accounts for around 85-90% of all cases of this medical condition.
Normally when you eat carbohydrates, they are broken down into glucose, which is transported through the body and taken up by your cells, where it is used as energy or stored for future use. Your body produces insulin, which is a hormone that helps the cells in your body absorb and use this glucose. Usually, your body regulates your blood sugar levels quite effectively.
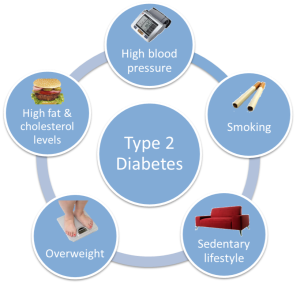
Type 2 diabetes is where the body starts to produce less insulin, or the insulin which is produced doesn’t work as well. The result is your body’s cells are unable to absorb glucose properly, and your blood sugar levels begin to rise. This form of diabetes is often caused by lifestyle factors such as having high blood pressure and high cholesterol, as well as being overweight, smoking, having a bad diet and not getting much physical activity. Those with a family history of type 2 diabetes are also have a higher risk of developing the condition. Type 2 diabetes is normally treated with oral medication, although some type 2 diabetics also require treatment with insulin.
High blood sugar, as a result of diabetes, can cause many problems. Short term, you may experience increased thirst and urination, blurred vision and fatigue. Over a longer period of time, uncontrolled high blood sugar can cause damage to blood vessels in the body, which can lead to kidney problems, a feeling of numbness in the feet (as a result of nerve damage), eye problems and heart troubles.
Type 2 diabetes also comes with a risk of low blood sugar, or hypoglycaemia. This can occur as a result of diabetes medications being a bit too strong, or simply not eating enough! Hypoglycaemia can make it hard to concentrate and carry out regular activities…..and if blood sugar levels drop too low, it can result in unconsciousness or even worse!
EXERCISING WITH TYPE 2 DIABETES
Exercise has many benefits, especially for those with type 2 diabetes. Regular physical activity can help improve the body’s response to insulin, which can help to keep blood sugar levels under control. Exercise can also help to improve other health conditions, such as high blood pressure, high cholesterol and weight problems; which in turn reduces the risk of developing even further problems as a result of their diabetes. By combining regular exercise with a healthy diet and weight loss, some people with type 2 diabetes are able to reduce the amount of medication they take. Quite a few people are even able to stop taking medication altogether…..you can’t get rid of type 2 diabetes, but with the right lifestyle changes, it is manageable without medications!
Of course, its always a good idea to have a chat to your doctor before you begin any exercise program. They will have a look at your blood sugar levels; and check to see if you have developed any other health problems as a result of your diabetes which may make regular physical activity a bit unsafe.
But while exercise and sports provide great benefits for diabetics, the short term and long term complications as a result of having diabetes can also pose a few challenges.
Many diabetics are at risk of developing foot problems, which can go un-noticed and take a long time to heal. Seeing a registered podiatrist can help with this, as they can advise on appropriate footwear; as well as giving advice on checking your feet and treating any problems which may arise.
The long term damage uncontrolled blood sugar can cause to blood vessels may eventually lead to heart problems. So, when you are out being active, if you experience any chest pain or discomfort, or any tightness or pain in your neck or arms, be sure to stop exercising. Its also important to stop exercising if you feel lightheaded, short of breath, or experience any other unusual feelings…..as these may be a result of heart trouble.
Unplanned physical activity, or a sudden increase in the volume or intensity of exercise can also cause hypoglycaemia. Its important to recognise the signs of hypoglycaemia early; so if you begin to experience any excessive sweating, shaking or trembling, dizziness or a lightheaded feeling, a sudden headache or pins and needles around the mouth, stop what you are doing and get some sugar into your system! Be sure to rest, eat a bit more food and keep a close eye on your sugar levels for at least the next 24 hours, to ensure the risk of hypoglycaemia is under control.
Close monitoring of sugar levels is of great importance for type 2 diabetics, especially when you are out exercising. Each individual’s diabetes is slightly different, and the way your body and blood sugar will react to exercise can vary greatly. The best thing you can do is begin any exercise regime slowly, monitoring your blood sugar levels carefully before, during and after exercise. Gradually build up the volume and intensity of your exercise…..ideally, you should be aiming for at least 30 minutes a day; but if you are aiming to lose weight, you may even build up to 90 minutes for each session! Remember, exercise can affect your blood sugar for up to 48 hours after you have finished, so make sure you are regularly checking your levels. The Accu-Chek Mobile* is a great meter for those heading outdoors on a regular basis, as it is basically an all-in-one unit which has a lancet attached, and doesn’t require any testing strips. It also allows you to download any data onto your computer, so you can keep track of your blood sugar levels as a result of your exercise.

When exercising, be sure to take appropriate supplies with you. Due to the risks of hypoglycaemia, ensure you have access to some form of sugar which can be absorbed quickly into your body, such as jelly beans or glucose tablets. Its also a great idea to have ready access to a Glucagen Hypokit, speak to your GP for a prescription for one of these. Remember to stay hydrated, and be sure to let everybody you are exercising with to be aware of your condition….they can keep an eye out for any signs of trouble!
For people who are involved with competitive sports, its probably worth knowing that some of the oral medications commonly used in the treatment of type 2 diabetes have previously been on the prohibited substances list. Although most are now okay to use, its always worth double checking here!
While type 2 diabetes can have some rather devastating long term effects, staying fit and healthy is one of the best ways of managing your condition! For more information on exercising and type 2 diabetes, have a chat to your GP. Dieticians, especially those educated in sports and diabetes, can help you manage your food requirement, you could contact Diabetes Australia to speak to a diabetes educator…..or feel free to leave me a message!
*Accu-Chek Mobile test cartridges are only government subsidised for those using insulin
(Disclosure statement – this is not a paid endorsement)


Ive cured so many type 2 diabetics by just cutting out their oil, animal product and any other fat content and increasing their carb content.
Works 100% of the time.
Big pharma and drug dealers like you dont like it cos they lose insulin customers haha.
No wonder you didnt give your type 2 readers the choice to self cure – you would NOT make any money from them anymore.
LikeLike
Hi Durianrider. I find your comments interesting. From all of the medical research I have come across, there is currently no known cure for type 2 diabetes. However, it is possible to manage type 2 diabetes without medications, through lifestyle modifications such as a healthy diet, regular exercise and weight management, as I have already suggested in my article.
I am also intrigued as to how increasing carbohydrates can “cure” type 2 diabetes (especially when medical research shows type 2 diabetes can only go into remission, not actually “cured”). Since carbohydrates will raise blood sugar levels higher and more quickly than any other nutrient (which is obviously unhealthy for a diabetic), I cannot see the medical reasoning behind this approach. Are there any peer reviewed, scientifically supported clinical trials available which support this management approach? I would be very interested to read them!
As for suggesting I don’t want to lose insulin customers, people with type 2 diabetes only begin to use insulin when all other forms of treatment, (including diet, weight, lifestyle modifications and oral medications) are unable to adequately control their blood sugar levels. As a responsible health care professional, nothing pleases me more than to see an individual improve their health to a degree where they no longer need medications to control any health problems they may have.
LikeLike
Hi,
A few comments;
1. “This form of diabetes is often caused by lifestyle factors such as having high blood pressure and high cholesterol, as well as being overweight…” might be overstating the case somewhat. These things are certainly associated with t2 diabetes, but are not necessarily causative. Multigenerational epigenetic factors are probably one of the more significant “causes” of t2 diabetes. (“Diabetes mellitus” is, strictly, a description of signs. Translation from Latin/Greek: “sweet urine”.)
2. Monitoring blood glucose levels is a useful management tool. How does my food intake need to be composed/balanced for my meal/snack following the reading?
3. My daughter (a t1 diabetic for 27 years) uses the Accu-Chek Mobile BG monitor you mention, and finds it much more convenient than the type of meter that I use (and she previously used). [I remember when she was first diagnosed, and the pain involved in extracting the HUGE drop of blood required for the early (optical) machines.] I use the Abbott “FreeStyle Neo” machine, partly because they (a spare for critical redundancy!) didn’t cost me anything. One was a manufacturer’s replacement for an outdated machine given to me by my daughter (since we suspected that for me it was not a case of “if” I developed t2 diabetes, but “when”); the other came gratis via a manufacturer’s cash-back offer and a favourable price from DiabetesSA. (Strips very cheap under NDSS.)
4. It would be very easy for a diabetic (t1 or t2) to get depressed by occasional runs of high BG readings. Blood glucose levels are also affected by minor illnesses, hayfever, the weather, and seasonally. (Anecdotal: higher readings in winter.) As long as overall control (as indicated by HbA1c) is satisfactory, no need to get upset. But, IF IN DOUBT, CONSULT A PROFESSIONAL, even if your friendly local pharmacist.
LikeLike
Hi David, thanks for the comments 🙂
Yes, you are right that genetic factors are a common link to type 2 diabetes, in addition to the lifestyle issues I have listed. Interestingly, the exact “cause” of type 2 diabetes is unclear, the genetic and lifestyle factors are more “links” that are common place in people with type 2 diabetes.
In terms of food, its hard to give an exact answer for everybody as to the balance/composition of what to eat after a reading, as there are so many variables involved (seriousness of type 2 diabetes, weight, is the reading high or low, how high/low is the reading, are you about to exercise or just finished exercising etc). Other than saying “have some sugar when low”, I apologise that this doesn’t really answer your question!
We are very lucky here in Australia with testing machines. The manufacturers regularly allow people to upgrade their machines cheaply (or often for free)….and the testing strips are very affordable when subsidised under the NDSS (Diabetes SA will soon be closing, but pharmacies will still serve as NDSS agents). I am looking forward to the day when continuous monitoring devices become subsidised and common place!
You are correct in saying that blood sugar levels can be affected by other illnesses and situations….speaking to a diabetes educator, your GP or local pharmacist is always a good idea if you have any worries 🙂
LikeLike