Type 1 diabetes accounts for roughly 10-15% of all cases of diabetes in Australia. Type 1 diabetes is an auto-immune condition which attacks the insulin producing cells within the pancreas. Type 1 diabetes usually develops in early childhood or adolescence….hence it is often referred to as juvenile onset diabetes.
In type 1 diabetes, the pancreas fails to produce enough insulin, or doesn’t produce any insulin at all. After eating, the body converts what we eat into glucose (amongst other things), which is transported through the blood, and taken up by the cells for use as energy, or to be stored for future use. Insulin is vital to this uptake process……so when the body fails to produce insulin, blood sugar levels rise, which can cause major health problems.
Over a long period of time, high blood sugar can result in health problems such as heart disease, kidney disease, nerve damage and eye problems. Type 1 diabetes also has the problem of hypoglycaemia, which is where blood sugar levels drop to dangerously low levels. This leads to individuals being unable to concentrate on every day tasks, and can result in a diabetic coma, or potentially even worse!
Treatment for type 1 diabetes relies on multiple daily injections of insulin, in combination with regular blood sugar level tests. Many types of insulin injections exist. They primarily fall into 5 main categories, depending on how long it takes for their actions to begin and how long they remain in the body.
Rapid acting insulin begins to work within 1-20 minutes. Its effects peak at around 1 hour, and can last for between 3 and 5 hours.
Short acting insulin works after approximately 30 minutes. It has a peak effect after around 2-4 hours, and continues to work for about 4-6 hours.
Intermediate acting insulin starts working after 90 minutes, with its peak effects after 4-12 hours. This insulin continues to work for about 16-24 hours.
Mixed insulin contains a combination of rapid or short acting insulin, mixed with an intermediate acting insulin. This is designed so type 1 diabetics can reduce the number of injections they need to give themselves over a daily basis.
Long acting insulin lasts up to 24 hours. This type of insulin provides the body with a background or base level of insulin to help regulate blood sugar levels across the day…..but type 1 diabetics still need to use a rapid or short acting insulin in addition to their long acting insulin.
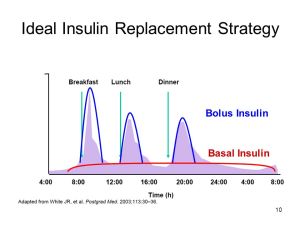
As every individual with type 1 diabetes is different, insulin needs vary greatly from person to person. People usually require a background level of insulin to work over the day (this is known as basal insulin), as well as regular injections of rapid or short acting insulin at meal times to help regulate blood sugar when larger amounts of food are being eaten (this is known as bolus insulin).
EXERCISING, SPORTS AND TYPE 1 DIABETES
Getting regular exercise is a great way to help people with type 1 diabetes manage their condition, as physical activity can improve the way the body responds to insulin. In addition, keeping fit can help to minimise and avoid the long term complications of type 1 diabetes. But one of the biggest problems with regular exercise for many type 1 diabetics is the fine balancing act required to keep blood sugar levels within the normal, healthy range. If levels are too high on a long term basis, it can lead to some major health issues. Too low, and a hypoglycaemic attack can occur, which is not a good scenario. But with the right knowledge, those with type 1 diabetes are able to excel at sports……..there is actually a professional cycling team (Team Novo Nordisk) whose riders all have type 1 diabetes!
Changes in exercise intensity and duration can affect the rate at which energy is used, and the extra carbohydrate intake required for exercise (both low and high GI) can sometimes make it difficult to control blood sugar levels. On one side of the coin, blood sugar can be increased by, among other things, a bit too much food, a reduction in exercise volume and intensity, or not quite enough insulin. On the other side, blood sugar levels can drop too low (sometimes resulting in hypoglycaemia) by not eating enough, an unplanned increase in exercise intensity and duration, or injecting a little bit too much insulin…..and to make things even harder, as each individual is different, there is no simple answer that will solve the equation for everybody!
So where to start? Well, knowing the needs of your own body is the most important thing!Checking your blood sugar levels on a regular basis is one of the keys to this…..the more often you check your sugar levels, the better you will know what your body needs! When beginning any new exercise program or activity, the best thing to do is start slowly. As you get into a routine with your exercise, you will gradually learn how your body reacts to physical activity. This will help you learn how to effectively manage your diabetes and keep your blood sugar levels in a healthy range. Likewise, if you are going to change the volume or intensity of your regular exercise routine, do so slowly, and increase how often you monitor your sugar levels.

Following a structured diet can help to keep your sugar levels where they need to be, and help avoid any potential problems. Have a read of my article on sports nutrition for a bit more information on what to eat and when if you are an active person….this may give you a good starting point. A sports dietician who has knowledge and experience with type 1 diabetes can also help you develop a good eating plan.
Always ensure to check your sugar levels before you start any exercise for the day. If your levels are a bit high, this is nothing to be concerned about, as they will come down as you are exercising. However, if your sugar levels are low, its probably best not to exercise at all….you will be putting yourself at risk of a potentially dangerous hypoglycaemic attack!
During endurance sports or exercise lasting longer than 1 hour, you will need to check your sugar levels during your activity……and as you will more than likely be eating during your exercise, you will probably need to inject a small amount of insulin every now and then too, so make sure you carry some with you!
Also be sure to check your blood sugar level directly after any physical activity, to ensure it is within a healthy range. Have some sugary food on hand in case your level is a bit low (you don’t want to risk a hypoglycaemic attack!), and make sure you have some insulin readily available, as you will want to be eating something after your sport or activity to help your recovery.
For the rest of the day, its a good idea to continue to check your blood sugar levels on a regular basis, especially after harder efforts or longer activities, as your metabolic rate may be raised for 24 hours after sports or exercise. If your levels were a bit low after exercising, regular checks will also reduce the risk of developing a hypoglycaemic attack later in the day.
Knowing the signs and symptoms of a hypoglycaemic attack is important. By learning what to look out for, you will be able to detect what’s happening nice and early, and treat any potential hypoglycaemic attack before it happens! Early signs of hypoglycaemia include increased sweating, trembling, hunger, feeling lightheaded or dizzy, a headache, and pins and needles around the mouth.
For any physical activity, regardless of length or intensity, be sure to have an emergency pack on hand. This should contain some sugary foods which can quickly be absorbed into your system, a GlucaGen Hypokit (speak to your GP for a prescription for one of these) and some insulin. Having a kit on hand will allow you to treat a hypoglycaemic attack if you experience one, and manage any high blood sugar readings you may have.
Some people may benefit from insulin pumps. Being about the size of a mobile phone, these are devices which remain injected; and provide a gradual “drip feed” of insulin over the day to keep basal levels where they need to be, as well as having preloaded doses of bolus injections which can be administered at the press of a button. But as they can be knocked around a bit and easily become detached, especially during contact sports, they are not for everybody.

Continuous glucose monitors are a great idea for those who exercise or compete in sports, as they provide constant monitoring and reporting of your blood sugar levels over the day. These types of devices are able to give more precise blood sugar level control, as they can give you early warnings of potentially high or low blood sugar level readings, and allow you act quickly. Unfortunately, this technology is rather expensive, but the Australian Government is developing a program to subsidise these devices for some type 1 diabetics.
For any athletes out there who are competing at an elite level with type 1 diabetes, it is worth knowing that insulin is on the WADA banned substances list. However, you will easily be able to apply for a therapeutic use exemption! WADA also has a policy where injections providing more than 50ml over a 6 hour period (unless needed due to hospital admission, surgical procedure or clinical investigations) are banned. Fortunately, insulin injections are well below this volume of fluid…..so you have nothing to worry about!
Of course, its a smart to let everybody around you know of your condition….they can keep an eye on you, especially if you start showing the signs of a hypoglycaemic attack! Make sure they know what they can do to help you, such as reminding you to check your sugar levels regularly, or carrying a bit of extra food for you to borrow if needed.
The most important thing to manage your type 1 diabetes, especially during exercise, is education. You will gradually learn exactly what your body needs and what to look out for. Speak to as many people to help you out as possible, such as a trained diabetes educator, a sports dietician who has experience with type 1 diabetes, your GP or even your local pharmacist. With the right knowledge and the right tools, there is no need for your type 1 diabetes to slow you down in any way!


My daughter (T1 for 27 years) uses a pump, and one of the afore-mentioned AccuCheck Mobile meters. She has a T-shirt which reads “My pancreas runs on AAA batteries”.
One of the often-observed side-effects of excellent control is weight gain. ):
The first time she went into the CBD, walking from home, after she was diagnosed, we found her staggering around in Vic Square about an hour later in a semi-conscious hypo state. (We were going to the Mall, and just happened to be passing at the right time.) Sat her down, and I ran (literally) to Coles for a bag of jelly beans. Since then, she has never gone anywhere without some jelly beans or similar with her.
We also had to use Glucagon once, when she got gastro (acquired in hospital!). Her husband has also had to use it a few times.
If one is a T1 diabetic, and one tends to easily slip into a hypo, it may be worth in some cases, carrying a glucagon kit, and having a trusted someone in one’s company know when and how to use it in an emergency.
LikeLike
Hi David….once again, thank you for your comments 🙂 As you have suggested, one of the smartest things a diabetic can do is have the resources available to treat a hypo, and make sure the people they associate with are able to help them in the event of one….it may just save their life.
LikeLike